What is Magnetic Brain Stimulation and How Does It Work?
Magnetic Brain Stimulation, a groundbreaking technique in neuroscience, is altering our understanding of brain functions. Dr. Emily Carter, a leading expert in the field, states, "This method opens doors to new treatments that were once thought impossible." The technique uses magnetic fields to stimulate nerve cells in the brain.
Patients with mental health issues may benefit significantly from Magnetic Brain Stimulation. It's a non-invasive method that has shown promise in treating depression and anxiety. The precise mechanism remains a topic of research. Some experts believe it can enhance neural connectivity, while others emphasize the need for further studies.
Despite its potential, there are challenges. Some individuals may not respond well to treatment. Questions linger regarding long-term effects, urging caution. As we explore Magnetic Brain Stimulation, it's essential to weigh its benefits against uncertainties. This balance may lead to more effective applications in the future.

What is Magnetic Brain Stimulation?
Magnetic Brain Stimulation (MBS) is an innovative technique that uses magnetic fields to stimulate nerve cells in the brain. It primarily employs transcranial magnetic stimulation (TMS). This non-invasive method can influence brain activity without any surgical procedures. According to recent studies, TMS has shown promise in treating conditions like depression, anxiety, and PTSD.
Research indicates that nearly 40% of patients report significant relief from depressive symptoms after multiple sessions of TMS. The repetitive magnetic pulses activate specific brain regions. These regions are often underactive in individuals suffering from mood disorders. However, results can vary. Not everyone responds positively to treatment.
MBS offers a new avenue for those who haven’t found relief through traditional therapies. Yet, the approach demands further scrutiny. The exact mechanisms remain partially understood. Some patients experience side effects, including headaches or discomfort at the site of stimulation. These complexities can affect overall satisfaction with the treatment. It remains essential to approach MBS with cautious optimism.
The Science Behind Magnetic Brain Stimulation
Magnetic Brain Stimulation (MBS) is an innovative technique that uses magnetic fields to influence brain activity. The science behind it is fascinating and complex. At its core, MBS targets specific regions of the brain, sending electromagnetic pulses. These pulses can stimulate neurons, enhancing or inhibiting their activity. This process can lead to improvements in mood, cognition, and even motor skills.
Researchers often use MBS for various conditions, including depression and anxiety. Studies show that MBS changes how neurons communicate with each other. For example, it can increase the release of neurotransmitters like serotonin. These changes can stimulate areas of the brain linked to emotional regulation. However, results aren’t guaranteed for everyone. Some may experience minimal benefits, or even adverse effects.
Despite its potential, MBS is not a one-size-fits-all solution. Each person's brain is unique, leading to varying responses. Perhaps, more exploration is necessary to fully understand its implications. Questions remain about long-term effects and optimal treatment protocols. The science of MBS is still evolving, requiring cautious optimism. With ongoing research, we may uncover deeper insights into its capabilities and limitations.
How Magnetic Brain Stimulation is Administered
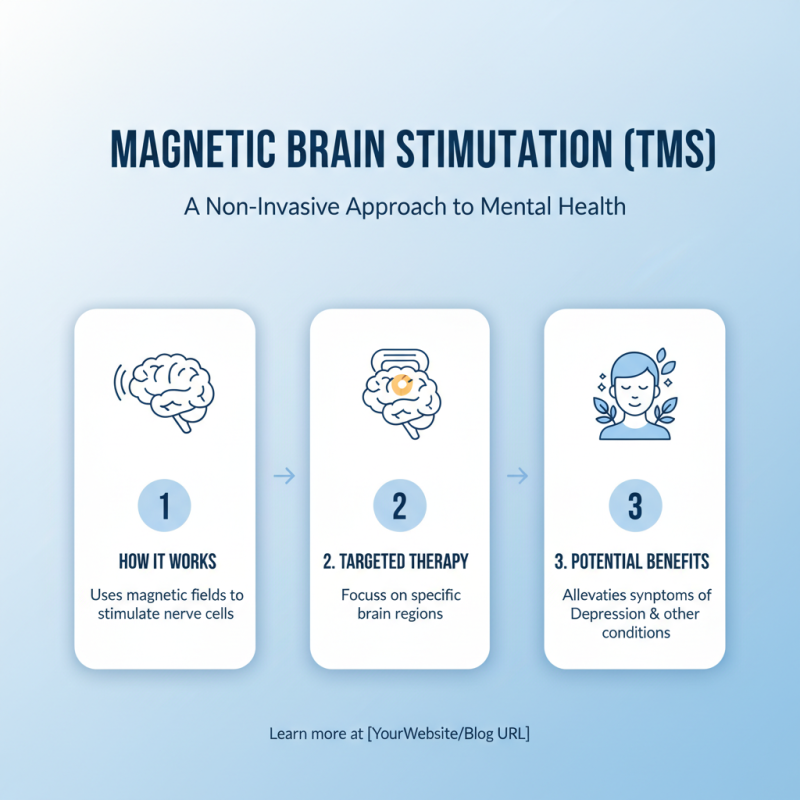
Magnetic Brain Stimulation, commonly known as TMS, is a fascinating procedure. It utilizes magnetic fields to stimulate nerve cells in the brain. This technique targets specific brain regions. By doing so, it aims to alleviate symptoms of various mental health conditions, including depression.
Administering Magnetic Brain Stimulation involves several steps. Patients typically sit in a comfortable chair. A coil is placed against their scalp. This coil emits magnetic pulses, which penetrate the skull. Each session lasts around 30 to 40 minutes. Patients may feel a tapping sensation on their head with each pulse.
During this process, some may experience mild discomfort. Others might find it relaxing. It's essential for practitioners to adjust the stimulation intensity based on individual tolerance. Post-session, individuals can usually resume their daily activities. However, some may need multiple sessions to notice significant changes. There is still much to learn about TMS's long-term effects, leaving room for improvement and reflection.
Applications of Magnetic Brain Stimulation in Medicine
Magnetic brain stimulation, particularly Transcranial Magnetic Stimulation (TMS), has gained traction in medicine. Research indicates that TMS can effectively alleviate depression symptoms in 50-60% of patients. This non-invasive method uses magnetic fields to stimulate nerve cells in the brain, promoting neural activity associated with mood regulation.
In addition to treating depression, TMS is being explored for other conditions. Studies suggest positive results in anxiety disorders and PTSD. A report from the National Institute of Mental Health highlights that TMS may improve cognitive function in patients with schizophrenia. However, more research is needed to confirm these findings and determine long-term effects.
Tips: Always consult a healthcare professional before considering TMS. Monitor how you feel during treatment. Not everyone responds the same way.
While TMS presents promising benefits, it's crucial to address its limitations. Some patients may experience discomfort or side effects like headaches. Understanding these drawbacks is important for informed decisions. The field of magnetic brain stimulation is evolving rapidly, but it's essential to approach it with realistic expectations and awareness of individual variation.
Applications of Magnetic Brain Stimulation in Medicine
This bar chart illustrates the number of clinical studies conducted in 2023 on various applications of Magnetic Brain Stimulation in medicine, highlighting its growing importance in treating various neurological and psychological conditions.
Potential Risks and Side Effects of Magnetic Brain Stimulation
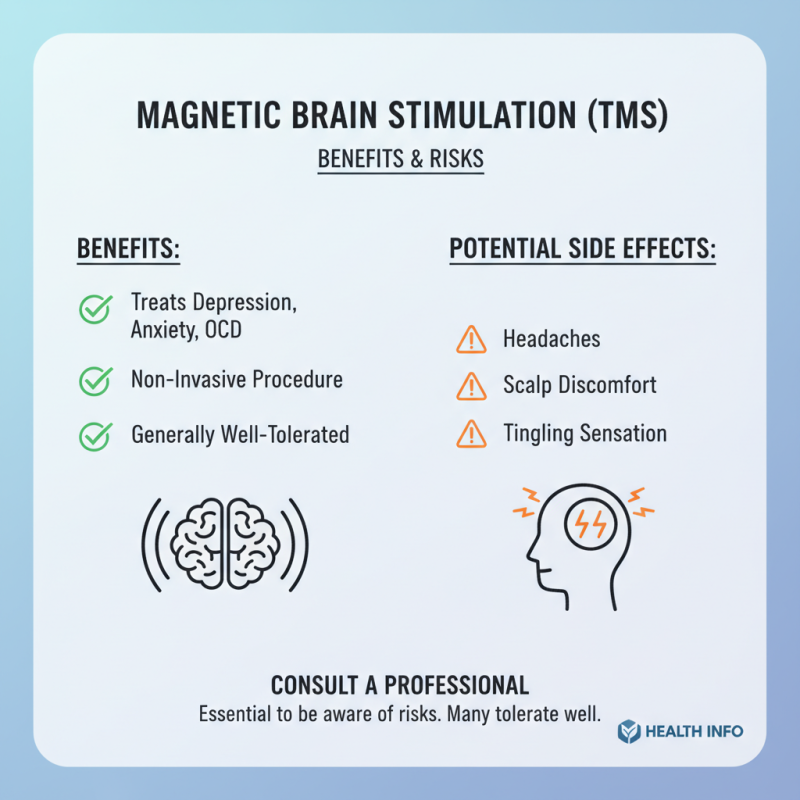
Magnetic brain stimulation is becoming more popular for treating various mental health issues. However, it is essential to be aware of potential risks and side effects. While many people tolerate the treatment well, some experience mild to moderate discomfort. This can include headaches, scalp discomfort, and a tingling sensation at the site of stimulation.
More severe reactions, although rare, can occur. Some individuals might experience seizures, especially those with a history of epilepsy. Additionally, some patients report mood changes or increased anxiety shortly after treatment. It's important to monitor these reactions closely and discuss them with a healthcare provider.
Not everyone will react the same way to brain stimulation. Individual responses vary significantly. The nuances of each person's brain and body mean that what works for one may not work for another. Keeping an open dialogue with medical professionals can help mitigate risks, leading to safer experiences for those seeking help.
Related Posts
-

What is Magnetic Brain Stimulation and How Does It Work?
-

Ultimate Guide to Unlocking the Benefits of Tms Magnetic Stimulation Therapy
-

Top 10 Manufacturers of Magnetic Brain Stimulation at the 137th Canton Fair in China
-

Unlocking the Future of Manufacturing with Best Rtms Machine and Strategic Innovations for 2025
-

Top 7 Benefits of Transcranial Stimulation for Mental Health Improvement
-

Exploring the Potential of Non Invasive Brain Stimulation for Enhancing Cognitive Function and Mental Health
